4.
Clinical Aspects

Bacterial Meningitis is generally preceded by upper respiratory tract illness in adults and children when the natural habitat is the different meningococcus bacteria’s that occur in the human nasopharynx. [40] It is a non-motile, gram-negative diplococci bacterium that transfers from one host to another via direct contact with body fluids and causes various symptoms. [42;47]
The patient has the most common form of Bacterial Neisseria Meningitis with clinical features of high temperature of 40 degrees, neck supplement, fever, and headache, which indicate inflammatory activation of the trigeminal sensory nerve in the meninges and presumably can be stopped by 5-HT1B/D/F receptor agonists. [43;44] (Figure 1)
However, the symptoms of BM are often non-specific, especially at young ages as the 19-year patient and can be challenging to determine. [46] Neisseria meningitidis bacteria multiply rapidly and lead to a mild subclinical infection. In approximately 10-20% of cases, the N.Meningitis enters the bloodstream called Meningococcaemia, which usually precedes the development of meningococcal meningitis by 24-48 hours. [45]
In some cases, the collapse of the blood vessels may lead to shock and called Waterhouse-Friderichsen syndrome, when the meningococcus bacteria spread to the blood due to septicaemia. [41] Later symptoms may include paralysis of one side of the body (hemiparesis), hearing loss, or additional neurological abnormalities.
The damage of the protective membranes covering the brain and spinal cord leads to bacterial or viral infection of the fluid surrounding the brain. [48,49] As a result, the spinal cord usually causes swelling occurring cerebral edema or ventriculitis, or hydrocephalus occurring accumulation of fluid in the brain cavity. [52] Additional symptoms may include chills, sweating, weakness; loss of appetite; muscle pain of the lower back or legs; or inability to tolerate bright light. [51]
Therefore, later determination leads to more complex, minor frequency symptoms of the meningococcal disease, including neck stiffness, photophobia, petechiae or haemorrhagic rash, altered mental status, myalgia, shock, and abnormal skin colour, purpura fulminans, or even disseminated intravascular coagulation (DIC). [50] (Figure 1)
Figure 1 The table of Frequency in percent depending on different symptoms of meningococal disease. Ref. Van de Beek D, Greeff SC, Melker HE, Schouls LM, MJ Thompson.[53; 54]
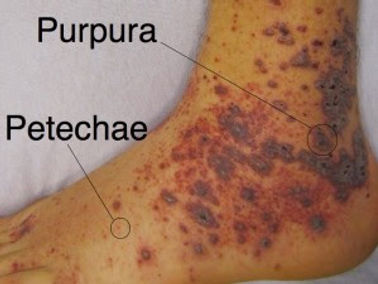
Although one of the characteristic rashes is a more specific finding, it is observed in only 45% to 65% of cases at presentation. [55;56]
In addition, meningococcal rashes depend on skin type and look diverse, continually developing into a non-blanching red, purple, or brownish petechial rash or purpura, meaning it will not go away when pressed. [58]
For example, when a petechial rash appears as red or purple patches on the skin and may resemble flea bites, while the purple rash looks more like a bruise, appearing as reddish-purple patches on the skin. [57] (Figure 2)
Bacteria invade the blood vessels and organs, causing damage to them while the result is followed by leakage of blood through vessels, appearing in rashes. [59]
Figure 2. The difference between 2 types of meningococcal rashes; Santistevan Jamie, MD; JUL 18TH, 2016 [60]
Furthermore, the low platelet counts (thrombocytopenia) and several platelet function disorders increase the risk of bleeding, while the white blood was represented bacterial infections by the increased count of white blood[61;62;63] Therefore, the clinical features of Meningitis are challenging to detect and depend on different factors as age, symptoms, types of rashes, and blood test examination.
Supportive material: Animator - Sunny Rai Intro created by Ilhaam Mullagee (Music -- Longzijun); https://www.youtube.com/watch?v=FHLWnlrmKNg
References
-
40. Vasudeva Shikha S, MBBS Assistant Professor of Internal Medicine, Virginia Tech Carilion School of Medicine; Nov 16, 2021; Meningitis
-
41.Kandola Aaron; 2020; The Journal of Medical News Today; What is a complete blood count?
-
42. Runde; Tyler J. 2021; Fatima Anjum; John W. Hafner; Illinois College of Medicine; Bacterial Meningitis
-
43. Diederik van de Beek 1, Jan de Gans, Lodewijk Spanjaard, Martijn Weisfelt, Johannes B Reitsma, Marinus Vermeulen; 004 Oct 28;351(18):1849-59. doi: 10.1056/NEJMoa040845; Clinical features and prognostic factors in adults with bacterial meningitis
-
44. Hoffmann O., Keilwerth N., Bille M.B., Reuter U., Angstwurm K., Schumann R.R.et al. (2002) Triptans reduce the inflammatory response in bacterial meningitis. J Cereb Blood Flow Metab 22:988–996
-
45.Rappuoli Rino NORD gratefully acknowledges, PhD, Global Head of Vaccines Research, Novartis Vaccines and Diagnostics, Siena, Italy, for assistance in the preparation of this report, Meningococcal Meningitis
-
46. Bashir H El, M Laundy, and R Booy; 2003 Jul; Academic Department of Child Health, Queen Mary School of Medicine and Dentistry at Barts and The London, 88(7): 615–620; Diagnosis and treatment of bacterial meningitis.
-
47. Nadine G. Rouphael and David S. Stephens, 2015 Mar 4; Neisseria meningitidis: Biology, Microbiology, and Epidemiology
-
48.Li Shan,corresponding author. Ivy P. Nguyen, and Kyle Urbanczyk; 2020 Dec; 10(12): 2227–2259.doi: 10.21037/qims-20-886; Common infectious diseases of the central nervous system—clinical features and imaging characteristics
-
49.Ragunathan L, Ramsay M, Borrow R, et al. Clinical features, laboratory findings and management of meningococcal meningitis in England and Wales: report of a 1997 survey. Meningococcal meningitis: 1997 survey report. J Infect 2000;40: 74–9.
-
50. Nash Anthony A., Robert G. Dalziel, and J. Ross Fitzgerald; 2015: 171–231.
-
51. Goel Anju, MD board-certified in internal medicine, September 10, 2021; Symptoms of Meningitis
-
52. Karki Bhesh R.; Yub Raj Sedhai; Syed Rizwan A. Bokhari; July 30, 2021; Waterhouse-Friderichsen Syndrome
-
Published online 2015 Feb 6. doi: 10.1016/B978-0-12-397188-3.00008-1; Mechanisms of Cell and Tissue Damage
-
53.Runde; Tyler J. 2021; Fatima Anjum; John W. Hafner; Illinois College of Medicine; Bacterial Meningitis
-
54.Thompson MJ, Ninis N, Perera R, et al. Clinical recognition of meningococcal disease in children and adolescents. Lancet 2006;367:397–403.
-
55. Greeff SC, Melker HE, Schouls LM, et al. Pre-admission clinical course of menin- gococcal disease and opportunities for the earlier start of appropriate interven- tion: a prospective epidemiological study on 752 patients in the Netherlands, 2003-2005. Eur J Clin Microbiol Infect Dis 2008;27:985–92.)
-
56. Nixon Nguyen; Derrick Ashong. October 12, 2021; Neisseria Meningitidis
-
57. Carter Katherine; March 2019; Meningitis Research Foundation; “What is the 'meningitis rash'?”
-
58. Barrell Amanda on January 27, 2021; Medical News Today; Causes for a non-blanching rash in adults and children
-
59.Wan Cordia, MD Adult Neurologist, Kaiser Permanente Hawaii, Kaiser Permanente Southern California; Jul 17, 2018, Chief Editor: Niranjan N Singh, MBBS, MD, Viral Meningitis Workup
-
60. Santistevan Jamie, MD (ED Quality and Administrative Fellow, University of Wisconsin, Edited by: Alex Koyfman, MD (@EMHighAK, EM Attending Physician, UT Southwestern Medical Center / Parkland Memorial Hospital); JUL 18TH, 2016; What’s that Rash? An approach to dangerous rashes based on morphology.
-
61. Biggers Alana Medically reviewed, M.D., MPH — Written by Markus MacGill on November 16, 2018; What are the causes of a low platelet count?
-
62.Hoffmann O., Keilwerth N., Bille M.B., Reuter U., Angstwurm K., Schumann R.R.et al. (2002) Triptans reduce the inflammatory response in bacterial meningitis. J Cereb Blood Flow Metab 22:988–996
-
63.Van de Beek D, de Gans J, Spanjaard L, et al. Clinical features, and prognostic factors in adults with bacterial meningitis. N Engl J Med 2004;351:1849–59.